1- Before The Surgery
You have been told you need part of your colon removed because you have cancer. You should already have your surgery scheduled. If you don’t, please call your doctor’s office and get the surgery scheduled. Even if you are afraid of what might happen, with cancer, it is not a good idea to wait.
Before you actually go to the hospital for your surgery, there things you have to do. You will get help with all of this.
You have to meet with your surgeon to go over the surgery and sign paperwork, if you have not done that yet. Your surgeon will explain the surgery to you. He should tell you exactly what procedure you are having. You will need to sign an “informed consent” paper. You know that you are having the surgery to remove your cancer and parts of the colon around the cancer. The surgeon should make sure you understand this.
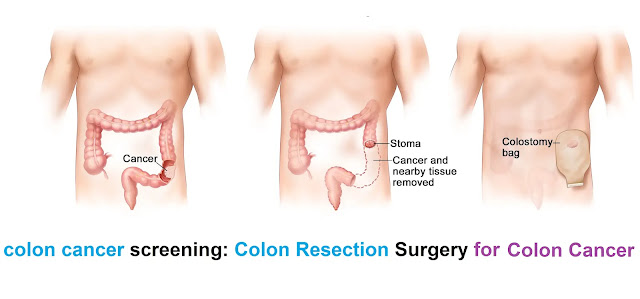
A colon resection can also be called a segmental resection or a hemicolectomy (half the colon is removed). It can be called a sigmoid colon resection if the surgeon plans to take out the sigmoid colon – if that is where your cancer is.
Your surgeon will tell you if he plans an open resection, which is the usual way to remove part of the colon.
Your surgeon might do a laparoscopic procedure. He can remove the cancer and parts of the colon using a laparoscopic procedure. But he will not be able to see everything inside your abdomen as well as with the regular surgery. If your surgeon thinks it is a good procedure for you, you need to know that with laparoscopic surgery:
- There are no large incisions.
- There are multiple small incisions.
- The surgeon uses a laparoscope, an instrument to see inside. The surgeon puts air inside your abdomen to keep the organs separate. He removes the cancer and parts of the colon through another small incision.
- You get better faster with this surgery.
Make sure and ask the questions you have. If there is something that frightens you, try and talk to the surgeon about it. Sometimes getting a question answered that was worrying you will make you feel a lot better. Some people are afraid of general anesthesia. You will meet the person who is going to give you your anesthesia probably just a little while before your surgery. But your surgeon can tell you that anesthesia now is very good and the side effects are much less than they were 20 years ago.
Sometimes, epidural anesthesia is used for this surgery. You may have heard the word epidural as pain control for women in labor. An epidural means that anesthesia is applied into the area around the spinal cord in your upper back. It is put in through a small tube that allows continued application. This works great – you feel no pain from the surgery. Most people still don’t want to be awake, so you get medicine to keep you asleep. Many surgeons do not use epidural anesthesia. If your surgeon and anesthesiologist do, talk about it. You will have less nausea after the surgery. Your intestines will start to work faster. You will probably go home sooner. Your pain control will be as good if not better than with traditional anesthesia. But the doctors at your hospital have to be skilled at doing this procedure.
If you are afraid of pain, your surgeon should explain to you that you will be able to get pain medicine when you need it. He should tell you how he gives his patients pain medicine. The medicine usually goes into the IV, or intravenous line, that you will get before surgery. Many patients get a system that they control. It is called PCA, which is short for Patient Controlled Anesthesia. You push a button to get more pain medicine when you need it, and it gets into the system very quickly. This is set up with a machine that prevents you from taking too much.
You should be told what the possible problems can be and what usually happens during and after surgery. The surgeon has to tell you about any bad possible outcome. He will have to mention death, not because he expects you to die, but because it is possible, very unlikely, but possible. In general, complications of surgery can include bleeding, infection, and trouble with the colon inside the abdomen. Please ask your surgeon any questions you have. Every surgeon is different. Every patient is different.
Your surgeon should also tell you what medications and vitamins you need to stop before the surgery, and when to stop them. He will tell you how to get ready for surgery. We will talk about that more in the next chapter.
People in your surgeon’s office may help you do insurance paperwork. Either your surgeon’s office or the hospital may contact your insurance company to get what is called “pre-authorization.” This means that the insurance company knows about your surgery and has okayed it.
You need to have a check-up before surgery. Your regular doctor, not your surgeon, will do your pre-op examination and tests. Your doctor will have to make sure you are well enough to have the colon resection surgery. That will mean he or she has to do a physical examination, to make sure your heart and lungs and other body systems can handle the surgery.
Your doctor will also order a number of tests. Most of the time, these tests are done at the hospital where you are going to have your surgery. They usually need to be done about 48 hours, or two days, before the surgery. The tests will include a chest X-ray and EKG (electrocardiogram – to check the heart) if you have not had these done recently.
You will also have a general blood panel done and your urine tested. This makes sure that your kidneys and your liver are working, that you do not have diabetes, and that your blood count is good. You may have a low red blood cell count. That is called anemia. You might have anemia because you have been losing blood from your cancer. You may need a blood transfusion during surgery, or you may need extra iron to build up your blood after the surgery.
It may be that not all of your tests are normal. You may have other medical problems. As long as they are being treated and the doctors know about them, you can still have surgery. Your regular doctor and your surgeon will know what medicines you need to take before, during and after your surgery. It is very common to have other medical problems.
Your blood will be typed so that if you need a blood transfusion, the very best blood for you can be used. If your blood count is already low, the hospital may even get blood ready just in case, the day of your surgery.
You will have to go to the hospital even if you don’t do tests there. You have to check in before the surgery. They will give you lots of forms to sign. They can be insurance papers, papers telling you your rights as a patient, papers telling the hospital who they can talk to about your medical condition. If someone calls to ask about you after surgery, no one will give out medical information unless you have said it is okay.
Someone at the hospital will ask you if you have made a “living will.” This means that they want to know what you want done if you stop breathing or your heart stops beating. Do not be afraid because they ask you about this. They ask every patient about this. It does not mean they think it is going to happen to you. You and your closest family members need to think about this. What do you want doctors and nurses to do if your heart stops? Do you want CPR (the short way of saying cardiopulmonary resuscitation) which means they try and pump the blood and breathe for you? Do you want electric shocks to try and restart your heart? If you have stopped breathing, do you want a breathing tube put in? Do you want to be connected to a machine that will breathe for you? There are no right or wrong answers for any of these questions. If you haven’t thought about them before, now is the time to think about them and talk to your family.
Once you have finished with all the paperwork, exams and lab tests, you will be almost completely ready.
2- Preparing for The Surgery
Before the surgeon works on your colon, he wants it to be cleaned out as much as possible. This chapter will give you a good idea of what to expect. Always follow the instructions of your doctor if there is a difference between what he or she says and the contents of this book.
Every surgeon has his or her own favorite method to clean out the colon. Usually you will stop your normal diet and start taking only clear liquids one day (24 hours) before your surgery. Some surgeons ask you to do this for two days. You will probably be given a laxative and/or an enema to clear all the contents out of your intestinal tract. Fleet’s enema or laxatives are often used. Other liquids to clean out the colon include GoLytely or Colyte.
If you cannot do this yourself, you may need to have it done in the hospital. Think about how you did before your colonoscopy. If it was very difficult for you, tell your surgeon. If you have no one at home to help you and you don’t feel well enough to do it alone, tell your surgeon. If you have many medical problems and take many medicines and the instructions confuse you, tell your surgeon. It is better to go into the hospital early and have your preparation there, than to get there and not be prepared.
Your surgeon should have already told you what medicines to stop and when.
All “blood thinners” must be stopped before surgery, usually five days beforehand.
Blood thinners can include:
- Aspirin, which you may be taking to protect your heart.
- Drugs to protect against stroke, like Plavix.
- Pain medicines like ibuprofen (Motrin and Advil), Aleve and all similar medicines. You might be taking these for pain of arthritis or other pain.
- Coumadin, heparin and warfarin. You may be taking these because you have had a blood clot in your legs, called a DVT (deep vein thrombosis). If that has happened to you before, your surgeon will need to take extra care to help prevent a clot after surgery.
- Many herbal preparations can thin the blood so you must stop all herbal remedies before your surgery. This can also be true with high doses of vitamins.
You will usually stay on all your other medicines up until the night before your surgery.
The routine is something like this: Start the clear liquid diet 24 hours before the day of surgery. Clear liquids mean liquids you can see through, that have no pieces of anything (like in soup) or fat. There are choices of clear liquids:
- Water is a clear liquid with no calories.
- Most clear fruit juices, like apple juice without pulp can be taken. Orange juice is not okay.
- Popsicles can be eaten.
- Jello can be eaten.
- Clear broth without anything in it can be taken. It may make a nice change after hours of sweet liquids.
- Gatorade may also be a good choice.
You usually need to drink 8 ounces of fluid every hour. Again, if you are on medicines that make you unsure if this is safe, please ask your doctor. Some time the day before surgery you will be asked to drink a laxative fluid like Fleet’s Phosphosoda. You might have to do this at two different times, at noon and in the evening. You should expect your bowels to empty. Eventually liquid should be passing through. Some doctors will add an enema at night to make sure the colon is clean. The idea is to have a clean colon without you getting too low on fluids and calories.
You will be told to take nothing by mouth after midnight, including water and medications. Your surgeon will advise you if you should take any of your medicines at midnight. Some surgeons may have you take an antibiotic at this time, but most do not.
This is all easiest if your surgery is early in the morning. That way you don’t have to be waiting for a long time without any food or water.
You will be told what time to arrive at the hospital. Someone needs to drive you. You need to bring what they told you to bring when you did your hospital paperwork. Leave valuables like your wedding ring and wallet at home. You will need your insurance card and your Medicare card. You will be wearing hospital gowns, but you may want a short robe from home for later. If you have a family member that can bring your things the next day, that would be great. You can pick out things you might want to read, or look at, as you are recovering in the hospital. You may or may not feel well enough to read.
3- In the Hospital Before The Surgery

You will be told when and where to go the day of your surgery. If you are already in the hospital, they will take you to the area where they get you ready for surgery. This is called the preop area (pre for before and op for operation).
If you had your prep in the hospital, you will already have an intravenous line giving you fluids.
What is an intravenous (IV) line? It is a tiny tube inserted into a vein, usually in your arm, but sometimes in the hand. It is hooked up to a bottle of fluids that usually has some salts and sugar mixed with water. The IV is put into your vein with a needle. Some nurses or health workers that “start IVs,” which is what they call it, use numbing medicine on the skin to reduce the pain of the needle. Whether they do or don’t, it is just a little pinch of pain. Once the tube is in, it should not hurt.
There are little side tubes off the main tube where nurses can inject medicine. There are some medicines that sting going in. They should tell you if they are going to give you something that stings. It stings only for a few seconds.
Most people come in the morning of the surgery. You will be asked to undress and put on a hospital gown. Your blood pressure, temperature, pulse, and oxygen level will be taken. They monitor the oxygen level in your system (and usually your pulse) by putting a clip on one of your fingers. It isn’t tight; it just feels a little strange. You will get used to it. You will have a blood pressure cuff around your arm that inflates and takes a reading. It could be every 15 minutes or every hour. It depends on where you are and what is happening to you.
Your intravenous line will be started. Blood may be taken at the same time, through the same tube, if there are any laboratory tests ordered by the doctor. You will have a specific nurse that assists you and maybe one or two other patients. This nurse will help you get ready, but will also be able to answer some questions and help calm any fears you are having about the surgery.
You will meet your anesthetist or anesthesiologist. That is either a doctor or a registered nurse with advanced training who gives the medicine to make you sleep through surgery. The anesthetist will go over your medical history, medicines, and ask if you followed the prep routine, especially not eating or drinking since midnight. If you have had anesthesia for anything in the past, he or she will want to know what you remember, good and bad.
You will probably be getting general anesthesia for your surgery. General anesthesia has changed a lot; much better anesthesia can be given now with less side effects. Ask any questions you might have. You will be getting a medicine to make you sleepy right before surgery.
If you have a family member with you, he or she will be asked to wait in the waiting room during some of this. Once you are settled, your family member can wait with you until it’s time to go into surgery. He or she should be there when you talk to the anesthetist and may be able to ask questions you did not think of.
Your surgeon will also come in and say hello. He will probably ask you if you completed your prep without problems. He will also probably tell you and your family member how long he expects the surgery to take. Your family can wait in the waiting room, and he will come out to tell them how you did at the end of the procedure.
Most surgeons order a dose of antibiotics given into your IV line an hour before surgery. This is to kill the bacteria in you colon.
Once you and the doctor are both ready, you will be moved on a rolling bed to the operating suite. If you wear glasses, they will be left with your family member.
4- The Surgery

When you arrive at the surgical suite, you will be lying on a bed, usually covered in blankets so you don’t get cold, with an IV in your arm for fluids and medicines, the clip on your finger and a blood pressure cuff.
The person who gives you anesthesia, who you have met already, is in charge of making sure that you are asleep and that your heart and lungs are doing okay during the surgery. You will have little round “EKG electrodes” attached to your skin. These send signals back to a machine to record your heart’s electrical activity. The anesthetist will make sure your EKG is coming through properly, that he can see you oxygen content and check your blood pressure with all the things you are hooked up to.
He will give you medicine into your IV tubing to make you sleepy. Sometimes the medicine can sting a little. Soon after that you will probably fall asleep. He will be giving you general anesthesia into your lungs, along with oxygen. It is his or her job to keep you asleep but with all your “vital signs” normal. There are medicines he will continue to put in your IV that keep you asleep. The gas you breathe in also helps keep you asleep.
If you are having epidural anesthesia, the anesthesiologist will have you lie on your side. He will find the spot in your upper back, and numb up the skin with novocaine-like medicine. After that, he will use a needle to insert a tube into the epidural space around your spinal cord. He will put anesthesia in. He will ask you if your legs are starting to feel cold. This means the anesthesia is starting to work. He will then give you medicine to make you go to sleep.
As soon as you are sleeping, the nurses will start cleaning the skin of your abdomen (belly) with an iodine solution. You will have a catheter placed into your bladder. This makes sure the bladder is empty so it doesn’t get in the way of the surgery. It also lets the surgeons know exactly how much fluid is coming out. Once the area is clean and sterilized, the surgery will begin. You will not be awake or remember any of this.
There are two ways to do a colon resection. Usually, the surgeon opens up the abdomen with a cut so he can see the cancer, and all of the colon. This allows him to see if the cancer has spread.
The other way is the laparoscopic surgery. One small cut is made to put in a tube that the surgeon uses to look inside. Another cut is for instruments to be passed inside to work. There is a tube put in to pass air into your abdomen. This separates all the things inside so the surgeon can keep your colon away from everything else. In this procedure, part of the colon with the cancer can be removed and the two sides of the colon joined back together. But the surgeon cannot see everything in the abdomen. It is easier to recover from this surgery, but when cancer is involved, it may be more important for the surgeon to see all of it. Your surgeon will have discussed this with you. Even if he starts with a laparoscopic procedure, if he needs to, he can switch to an open procedure.
In an open surgery, the surgeon will make a cut across your abdomen in order for him to see everything. He will look around inside, find the colon and find the cancer. He will try and see if there appear to be any other spots of cancer.
Your surgeon will remove the cancer. He will also remove normal-appearing colon on either side of the cancer, to make sure he gets all of the cancer. The ends will be temporarily sealed closed as he removes the cancerous portion. After that, he will attach the two open ends to each other with sutures (stitches) or staples.
Your surgeon will check your entire colon for any visible evidence of cancer. He will take out lymph glands in the area to check to see if there is any cancer in them. If all of this goes well, your colon will be reconnected and the abdomen will be closed back up. Everything he has taken will be sent to the laboratory to check for cancer. You will have more antibiotics put in through your IV during surgery.
What else can happen?
- The surgeon might find evidence of more cancer. He will take out as much as he can. If he cannot remove it all, other plans will be made after surgery.
This is probably not going to happen since you have had scans before the surgery.
- He might decide, because the tissue of your colon is not perfect, that he cannot connect the two ends now. He might pull the end connected to your upper intestines out through your abdomen. This is called a colostomy. In almost all cases with colon cancer, this is temporary. There will be a second surgery to connect the ends back up.
- If you are having any trouble that the anesthetist detects, like low blood pressure or a pulse that is too fast, you might need more fluids, or medication. If you have lost a lot of blood during the surgery, you may need a blood transfusion.
This surgery usually takes about 3 hours. When the surgeon is done, you will be taken to the recovery room. When you wake up you will have your intravenous line in your arm, an oxygen mask or oxygen given to you by prongs in your nose. You will have a catheter in your bladder. You may also have a tube coming out of your nose that goes down to your stomach. This is to remove the normal stomach fluids so your intestines can rest.
5- After Surgery
You will probably have pain. The pain comes from where the surgeon cut through your abdomen. The nurse will ask you how bad your pain is, on a 1 to 10 scale. Think about this before you go to the hospital. Have you had bad pain already? Have you ever had a pain you would call a 1, a 5, or a 10? This is based on your pain, how much pain you can handle. There is no right or wrong answer.
If you had the laparoscopic surgery, you will have less pain. There is also a different pain you get from the air they have to pump into your abdomen. There is still some pain from the small cuts.
If you had an epidural, you may not have any pain until it wears off. That might take 12 to 24 hours.
You will be able to get medicine for pain. Each doctor sets things up differently. In the recovery room, you may have to ask for a pain shot. Then the nurse can put pain medicine right into your IV line. You may have a PCA pain medication setup already, or you may get one later. This is when you get to control your own amount of pain medicine. You have a button to push if you need more pain medicine. There is a safety which prevents you from taking too much. If you push the button for pain medicine as soon as you need it, you never have too much pain.
You don’t have to worry that you won’t get pain medicine. This might not be set up until you are in your hospital room. You can ask for it as soon as you need it.
In the recovery room, they will make sure you wake up and are doing well after the surgery. They will check all the things like blood pressure a number of times. They will talk to you to see how you feel. They will look at your belly where the cut was made.
Usually one family member at a time can come into the recovery room. You may not remember all of this because you still may be sleepy. The surgeon may talk to you. He will definitely tell your family how the surgery went, so you can ask them later.
Some of the tubes may bother you. The tube in the nose can be very irritating. It can make it difficult to talk. Eventually all of the tubes will be removed.
You will stay in the recovery room until the nurse thinks you are doing well enough to go to your room. You will not be watched as closely in your room, so if there is anything of concern you will stay in the recovery room until you are stable.
Once you do get to your room, you will probably have a roommate. This can be difficult. It is very common for people in the hospital to get confused. Your roommate may get noisy or upset. The same thing might happen to you, but you can try to stay calm. There are curtains to draw around your bed for some privacy.
Here are some problems and some solutions:
- Pain from the surgery. Be sure and get pain medicine you need. Do not try and “tough it out.” It will only get worse. It has been proven that it is easier to control pain by taking medicine regularly then waiting until pain gets really bad. Use the PCA if you have it. If your doctor prefers to give you regularly scheduled pain medicine, take it. If you have medicine ordered for severe pain when your regular medicine isn’t helping, and you have severe pain, ask for it. You must have enough pain medicine to do the things you need to do to recover.
- The tubes bother you. You are kind of stuck with these for awhile. The tube into your bladder may come out first. If you seem to have plenty of urine, if you are awake and feeling strong enough, and you think you might be able to go on your own, it can be taken out. But remember, getting up to go to the bathroom or to use a bedpan or a potty chair is going to hurt, so you may need pain medicine.
- Your mouth is dry but they won’t let you drink. Try ice chips. There are also little sticks to wipe your mouth that give some moisture.
- You are getting a little confused about what is going on. This is something to talk about with your family and your doctor before you go to the hospital. Bring something from home to have by your bed. Make sure you can see a clock. Ask for help if you need it. You may want a family member to stay with you as much as possible. If you have family members who are willing to stay with you, let them, as much as the hospital allows.
- They keep waking you up to take your blood pressure and temperature. Unfortunately, no one ever sleeps well in the hospital. You need to get better so you can go home.
- The nurse doesn’t come in when you push the button for nurse. Or your medicines don’t arrive on time. Or you are unsure if you are getting the right medicine. This can be a problem in some hospitals if there aren’t enough nurses. Again, if someone can stay with you, ask them to help you. They can take a look at your medicines and get the names. They can make sure you are getting what the doctor ordered. They can walk out of the room and find a nurse.
If the surgeon had to give you a temporary colostomy, you will have to learn how to take care of it. Your family can help. If you have a colostomy, gas and stool (poop) will come out of that area on your abdomen, into a bag. You will not have anything new coming through your rectum and anus. Later on, surgery will reconnect the two ends of your colon.
There is also the gas pain you get if you had laparoscopic surgery. Sometimes you can feel it move around. Sometimes you feel pain in your shoulders. Ask the nurse for help with this pain.
Your surgeon will see you every day in the hospital. You can ask questions. He will be able to give you some news about the surgery. He can tell you if he thinks he removed all of the cancer. He can tell you if was able to connect the two ends of your colon. He can tell you if it looked like the cancer had spread. He can tell you if he thought the lymph glands looked normal.
The doctor will not be able to give you any definite information about the stage of your cancer yet. The pathologist has to look at all the samples under the microscope and do tests. This takes days to weeks.
Some people want to leave the hospital too early. Some don’t mind the hospital. Most people want to go home, to sleep in their own bed as soon as they can. Here are the things you have to do before you can go home.
- Your intestines have to wake up. They will start to make sounds, called bowel sounds. They may sound or feel to you like your stomach is rumbling. Eventually you will pass gas. That means you will fart! That will be a big deal. If you have had a tube in your nose, it can come out.
- You have to start taking something by mouth. This starts with small amounts of liquids. You have to see how your intestines do with anything that goes in. If you have bowel sounds and you are passing gas, they will start to give you something to eat. After the liquids, you will get soft, bland food. If your body isn’t ready, you might throw up, or you might have more pain. But eventually things will start going through.
- You have to get up and walk. You have to try this the first day. Even if you only make it as far as a chair next to your bed, you have to try. If you don’t get out of bed and you don’t walk, you can have more problems. You can develop areas in your lungs that don’t work. You can get blood clots in your legs. Walking is needed for good circulation. Walking also helps get your intestines working again. You even have to walk with the tubes. It will help you get rid of the tubes.
- Your lungs have to be working. You need to learn to breathe deeply even with the pain. They will give you a gadget to blow into. It will show you if you are working hard enough.
- You have to be able to pass gas easily, and maybe even stool. It may look different than what you are used to.
- Your pain must improve to the point that medicine in pill form controls it enough.
To review, in order to go home you have to:
- Be able to eat and not vomit.
- Be able to pee on your own.
- Be breathing well.
- Be passing gas and maybe stool through your rectum (you have to fart and maybe poop). If you have a colostomy, it needs to be functioning and you have to learn how to take care of it.
- Be able to walk up and down the hall.
- You have to be able to manage on pain medicine taken by mouth.
All of this takes a bit of time. If you had a regular abdominal surgery you will be in the hospital a number of days, anywhere from three to ten days. With the laparoscopic surgery, you may be able to go home in two to five days. The pain is significantly less and everything starts working again faster.
If you have other medical problems, your regular medicines will be given to you while in the hospital. Other medical problems can slow down your recovery.
6- Going Home
On the day you leave, someone has to drive you. That person should also pick up prescriptions you are going to need. You will need to be taking a stool softener, because pain medicine can cause constipation. You will need pain pills. You will need all your regular medicines. Other medication depends on how your surgery went.
Once you are out of the hospital, problems can develop. Some problems are very important. Your surgeon will give you instructions. Generally you should call your surgeon if:
- Your pain starts to get significantly worse instead of better.
- You start to run a fever.
- You see increasing redness, or drainage from surgery area.
- You see anything like pus or blood.
- You have intestinal symptoms that are new, or getting worse, including constipation, vomiting, -blood in the stool, or black tarry stools.
- Your abdomen puffs up like food is not going through.
- You feel very unwell and you don’t know why.
You will have an appointment scheduled with the surgeon in two to three weeks. At that time, he should be able to tell you the stage of your tumor, and whether or not you will need more treatment. Chemotherapy or radiation therapy is often used even with a very successful surgery. This is to make sure there are no cancer cells left anywhere.
At home, you have to recover. You will need to find a balance. Don’t do too much, but don’t do too little. You need to walk every day. It should get easier. Your pain should be decreasing little by little. You should be getting used to how your colon is working now, which will be different than it did before surgery. Most people want to stay at home near a toilet. They don’t know how quickly they might need to get to the bathroom to poop.
You should not be doing anything strenuous, or anything using your abdominal muscles. Most patients lose weight as well as strength. It can take a couple of months for you to feel closer to normal. If you had the laparoscopic surgery, you may feel better in weeks instead of months.
7- What Comes Next

What comes next depends on the stage of your colon cancer. It is very common to have radiation therapy after colon resection surgery. Sometimes you get chemotherapy after surgery. This is to make sure there are no cancer cells left.
If the surgeon thinks he removed all of the cancer, your chances of a cure are very high. If you have Stage 1 colon cancer, your long-term survival after surgery is around 96%. If you have Stage 2 colon cancer, your long-term survival with just surgery is 86%. If you also have chemotherapy, that number goes up another 2 to 4 points, so 88% to 90%. Even in Stage 3, there are combinations of treatments that can keep you healthy for many, many years.
If your tumor has already spread, there are still many treatments that can help you. New ways to treat colon cancer are being discovered all the time.
Colon resection is almost always the center of the treatment. Once you have healed from your colon resection surgery, you are well on your way toward recovery from colon cancer.







.webp)


.webp)

Social Plugin